The MDU regularly supports members working privately as radiologists who have been notified of a clinical negligence claim against them. While claims are less frequently made against radiologists than consultants working in some surgical specialties such as orthopaedics or cosmetic surgery, they remain relatively common and compensation can exceed a million pounds. Managing known risks linked to clinical negligence claims is important both to protect patients and to avoid claims being brought.
Compensation costs
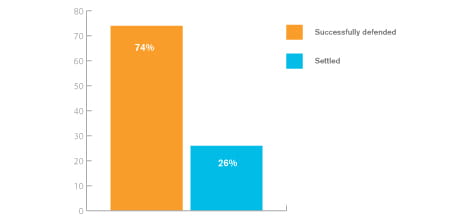
This analysis is based on 200 recent claims brought against consultant radiologists working in the independent sector who are MDU members. Nearly three quarters of claims were successfully defended with compensation paid in only around a quarter of cases.
Of the cases that settled, payments to cover compensation and legal costs varied widely, from just over £4,000 for a concerning report being issued to the wrong patient and causing them anxiety, to almost £2 million in a case where it was alleged terminal cancer had been missed. The majority of settled cases cost well in excess of £50,000.
The levels of compensation paid in clinical negligence claims bear little or no relation to the seriousness of the clinical allegations. Instead, they reflect the cost of restoring the claimant to the position they would have been in if the negligence had not occurred.
When large payments are provided to patients, much of the compensation paid is to fund the future care of badly injured patients or to compensate them for loss of earnings. These figures demonstrate the need for radiologists to have appropriate indemnity arrangements in place, as even the lower value claims can settle for damages and costs that are beyond the means of most members to pay.
It can be very distressing to find out a patient is bringing a claim against you. If you face a claim, you can be assured that the MDU’s expert claims handlers and medico-legal advisers understand how stressful this is and the importance of mounting a robust defence of your position. The MDU will defend claims whenever possible. We involve members in the conduct of their cases and will always seek your consent to settle a case.
While claims numbers have remained steady in recent years, the cost of claims has spiralled. This is not due to clinical standards, but to a deteriorating legal environment which the MDU is campaigning to reform.
Outcome of cases
Claims that were not settled were either discontinued by the claimant or statute barred (out of time).
Cases were discontinued because either the MDU successfully argued that liability should rest with treating clinicians rather than the radiology member, or the radiologist’s interpretation was reasonable in light of the clinical information, or did not alter the outcome for the patient.
A claim is statute barred if the claimant fails to bring a claim within three years from the date of the incident or the date of their knowledge of the alleged harm. This restriction does not apply to children with capacity, for whom the limitation period begins at 18 (16 in Scotland). There is no time limit for patients who lack capacity to conduct their own affairs.
Some claims were closed after the MDU successfully argued the member was not sufficiently involved in the clinical sequence of events.
Figure 1 shows the outcome of claims.
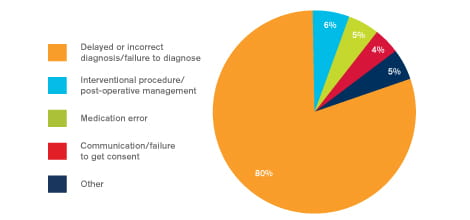
Reasons for claims
Delayed diagnosis
The most common condition involved in delayed diagnosis claims was cancer, which accounted for about a quarter of cases. Other conditions commonly resulting in a claim being made were fractures and cauda equina syndrome.
It is often argued that if an abnormality on an investigation had been recognised and/or reported correctly, then the patient would have been able to receive treatment for a condition sooner, thereby reducing the amount of disability that they had sustained.
Allegations usually centre on an abnormality not being detected, but in some cases it was alleged that an abnormality was picked up but misinterpreted, leading to unnecessary or incorrect treatment.
Medication issues
In a small number of cases, the main allegation was about a medication issue such as allergic reactions or providing the wrong medication. One claim involving the use of contrast in a child was settled for well over £100,000 with substantial claimant’s legal costs.
When a claim is settled and damages are paid, the MDU is also required to pay the claimant’s legal costs. These relate to the complexity of the case and the time it has taken to investigate. However, the costs can be disproportionately high and significantly exceed the amount of damages paid, as in the case mentioned.
Communication skills
A number of cases focused on the communication skills of the doctor, often when getting appropriate consent for a radiological procedure.
Interventional radiology
A few claims involved a substantial interventional radiology element, some of which were expensive to settle. Although interventional radiology is perceived to carry more risks, it is still far less commonly carried out then general radiology. It may also be that MDU members are more aware of the risk of interventional radiology and are justifiably cautious when undertaking these complex procedures.
Remember that certain risks, such as incorrectly reporting a radiology investigation, or communicating the recommendations following an investigation to the managing clinical team, are common to all types of radiological assessment.
MRIs and X-rays
Around a quarter of claims involved an MRI scan and a similar proportion involved allegations in relation to plain X-rays. In around 10% of cases, the claim followed the death of a patient.
Figure 2 shows the commonest reasons for claims.
Manage the risk
Claims involving radiologists often focus on a few key areas such as delayed or incorrect diagnosis. However, there are some common risk factors, which if managed appropriately, can help to reduce risks.
- Ensure robust procedures are in place for communicating results to relevant parties, to ensure appropriate and prompt follow-up and treatment.
- Be aware of the GMC’s guidance on consent and other relevant guidelines, such as those from NICE.
- Consent should be obtained by an appropriate member of the team and, ideally, by the radiologist undertaking the procedure.
- Ensure the patient is aware of the risks, benefits and complications of the proposed procedure as well other therapeutic options. These should be carefully documented.
- Supporting information such as patient leaflets and information sheets can help patient understanding. The use of these should be documented in the records.
- Consider the patient’s past medical history, medication history and allergies before administering pre-procedural medication and contrast media.
- Ensure appropriate handover to recovery staff for interventional procedures or those under sedation.
- Offer a chaperone to patients undergoing any intimate examinations, for example pelvic ultrasound.
- Consider contacting the referring doctor if you find something unexpected or which needs urgent investigation.
- Have a system in place to verify the right site and patient undergoing treatment and to cross check information provided against the referral.
- Ensure interruptions in the reporting room are kept to a minimum.
- If things go wrong, be open and honest with the patient by providing an explanation of what has happened and the likely short and long term effects of this. Say sorry and get advice from the MDU if you believe the incident triggers the organisations’ duty of candour requirements.
Case study
Ruptured Achilles tendon
A patient developed a pre-Achilles tendon bursitis and was referred for a steroid injection. The patient saw a radiologist MDU member, who had a special interest in ultrasound guided injection treatment.
The member undertook scans and discussed the procedure with the patient. The injection treatment was administered successfully, but three months later, the patient suffered a recurrence of the same symptoms again and saw a consultant rheumatologist.
The rheumatologist referred the patient back to the radiologist, who found a persistent left pre-Achilles bursitis.
After further scans the radiologist again obtained verbal consent for the procedure. A further steroid injection was performed, this time deep to the paratenon of the Achilles tendon. Shortly after the procedure, the patient left hospital and suffered a full thickness Achilles rupture.
The radiologist was notified of a claim. The solicitors’ letter alleged that on the balance of probabilities the rupture of the Achilles tendon was the result of injecting local anaesthetic and steroid around the tendon on two occasions. It was also alleged that the patient was not warned about, and wasn’t aware of, the risks of tendon rupture before either of the procedures.
An independent radiologist expert report was obtained by the MDU. The expert’s opinion was that the procedure was relatively safe and the member’s treatment was reasonable and logical. The expert also commented that the published evidence of outcomes following corticosteroid injection of the Achilles tendon suggests that the risk of rupture is around 1:1,000. The expert pointed out that the patient was referred for the procedure by a senior consultant rheumatologist, who also advised that this was an appropriate course of treatment.
Although the radiologist said a discussion with the patient about risk and benefits took place, this wasn’t documented. The expert remarked that there was no evidence in either of the ultrasound reports that the patient was consented for the risk - albeit a small one - of rupture.
MDU response
Based on these findings, the MDU denied liability on behalf of the member. However, the patient’s solicitors issued and served proceedings alleging that the radiologist did not seek consent from the patient for both procedures.
The radiologist agreed that despite verbally warning the patient of the risks and benefits of both procedures, this hadn’t been documented. With the member’s consent the claim was settled without admission of liability.
Damages were agreed at £12,500, but the legal costs were settled for almost five times that amount.
This page was correct at publication on 19/11/2019. Any guidance is intended as general guidance for members only. If you are a member and need specific advice relating to your own circumstances, please contact one of our advisers.
by Dr Shabbir Choudhury Senior medical claims handler
MBBS, DRCOG, DFFP, MRCGP, MA
Shabbir graduated from St George's University of London in 2002, qualifying as a GP in 2007. In 2010, he completed his MA in Medical Ethics and Law at King's College London. Shabbir continued to practice as a GP, and teach primary care ethics, until he joined the MDU in 2014. His main interest is the law and ethics of good Samaritanism.